- Home
- Join Our Campaign
- Epidemic of Hospital Harm

The Unhealthy History of Avoidable Hospital Harm
Hospital harm is the third leading cause of death in the United States and Canada, taking the lives of hundreds of thousands of patients every year. Many times that number are injured and often left severely disabled. The principal causes of these deaths and injuries are medication errors, hospital-acquired infections, falls, blood clots and pressure ulcers (bed sores), almost all of which are avoidable. In any year, hospital harm in the U.S. and Canada takes more lives than the combined toll of strokes, Alzheimer’s disease, kidney disease, breast cancer, and passenger train, airline and automobile accidents.
Government leaders, healthcare professionals and policy makers have known about the risks of hospital care causing preventable injuries and deaths for well over a decade. In 1999, the U.S. Institute of Medicine (IOM) released a ground-breaking report that warned:
Health care in the United States is not as safe as it should be — and can be. At least 44,000 people, and perhaps as many as 98,000 people, die in hospitals each year as a result of medical errors that could have been prevented, according to estimates from two major studies. Even using the lower estimate, preventable medical errors in hospitals exceed attributable deaths to such feared threats as motor-vehicle wrecks, breast cancer, and AIDS.
Hospital Harm Has Increased Over the Years
Recognizing that “the know-how already exists to prevent many of these mistakes,” the report set a minimum goal of reducing hospital errors by 50 percent over the next five years. Not only was that target not met, but the number of medical mistakes substantially increased. By 2010, the Office of Inspector General for the Department of Health and Human Services said that bad hospital care contributed to the deaths of 180,000 patients in Medicare alone in any given year. More research led to the discovery of even higher numbers.
As difficult as these numbers are to comprehend, when hospitals are subjected to a more rigorous review of deaths and adverse outcomes, like the kind using the “Global Trigger Tool” (instead of hospital self-reporting), the numbers in every case become stratospheric, suggesting that adverse events in hospitals may be ten times greater than previously measured. In 2013, the number of avoidable deaths from hospital harm in the United States had been estimated to be up to 440,000, according to the work of John T. James. His methodology and conclusion were endorsed by Dr. Lucian L. Leape, renowned as the father of the patient safety movement worldwide. In 2014, a committee of the United States Senate adopted the figure set by Dr. James.
Canadian estimates cite a minimum of 30,000 patients (UHN, 2015) killed each year from medical errors in the hospital setting. That’s the equivalent of one fully loaded jumbo jet crashing and killing everyone on board every week. Some researchers puts that figure considerably higher. A more recent Canadian study, which did not include the province of Quebec, reported that 1 in 18 hospitalized patients experienced avoidable medical errors in 2014 – 2015. In the U.S., it is estimated that 15 million incidents of hospital harm occur every year. In what other field of human activity are such regularly occurring disasters permitted?
Precise figures on hospital deaths and medical errors are difficult to obtain, given the voluntary nature of hospital reporting and the fact that, in many cases, hospitals simply don’t report when things go wrong. As Daniel R. Levinson, Inspector General of the U.S. Department of Health and Human Services, noted in a report of hospital care of Medicare patients:
Hospital staff did not report 86 percent of events to incident reporting systems…Further, hospital staff reported only 2 of the 18 most serious events in our sample (i.e., those events that resulted in permanent disability or death). Serious events not captured by incident reporting systems included hospital-acquired infections, such as a case of septic shock leading to death; and medication-related events, such as four cases of excessive bleeding because of the administration of blood-thinning medication that also led to death. Incident reporting systems did not capture any of the five NQF Serious Reportable Events and only one of the eight Medicare HAC events in our sample. Despite the existence of incident reporting systems, hospital staff did not report most events that harmed Medicare beneficiaries. Indeed, some of the most serious problems, including some that caused patients to die, were not reported. (Emphasis added.)
Nothing Like the Impact of Hospital Harm is Tolerated Anywhere Else in Society
This is an epidemic, any way you slice it. Would we tolerate this level of deaths and injuries associated with airline or railway accidents? If food poisoning were causing a fraction of the number of deaths that occur from hospital harm, would we remain passive? Would we allow our public leaders to remain indifferent?
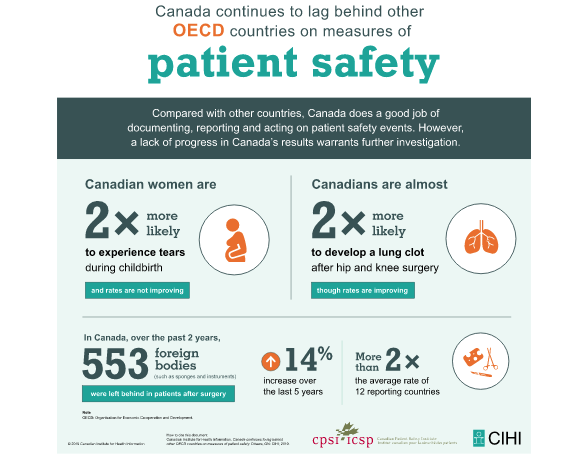
In the United States, more than 4,000 errors occur in the operating room every year. These include surgery on the wrong limb, on the wrong site of the body, and on the wrong patient, as well as “foreign bodies,” like towels, sponges and surgical instruments, left inside the patient during an operation. Canada’s record for leaving foreign bodies inside patients is the worst of all G7 nations, according to the Organization for Economic Cooperation and Development. Canada has also set the record for lacerations and punctures during hospital surgery.
 Infections pose another serious risk to hospitalized patients. They come in a variety of forms and have a number of different sources and causes. Their common connection is that they are all acquired inside the hospital. They all place patients at risk. And they all add to the costs of healthcare. Usually, they are avoidable. Hospital-acquired infections have been a problem for some time. But the shocking facts are that some one million patients in U.S. and Canadian hospitals acquire these infections each year, and up to 100,000 die as a result.
Infections pose another serious risk to hospitalized patients. They come in a variety of forms and have a number of different sources and causes. Their common connection is that they are all acquired inside the hospital. They all place patients at risk. And they all add to the costs of healthcare. Usually, they are avoidable. Hospital-acquired infections have been a problem for some time. But the shocking facts are that some one million patients in U.S. and Canadian hospitals acquire these infections each year, and up to 100,000 die as a result.
Canada’s Poor Record for Controlling Hospital Infections
In Canada, one-in-nine patients will acquire an infection as a consequence of their hospital stay. On that basis, it is Canada’s fourth leading cause of death. Canada’s infection control rate is one of the worst in the industrialized world, according to the World Health Organization.
The poor rate of hand hygiene compliance among healthcare providers in the hospital setting is a major reason for infections being able to quickly spin out of control. Most hospitals are far from 100 percent compliance in hand hygiene before and after patient contact. The figures provided are based on hospital self reporting that is not verified or externally monitored.
Awareness, Transparency, Accountability Keys to Combating Hospital Harm
Fortunately, there are exceptions to the situation described above. Many hospitals do superb work, are driven by a culture of patient safety and gifted with men and women who are a credit to their professions. These hospitals are working hard to combat this epidemic because they know that harm on the present scale is neither inevitable nor tolerable. It can — and must — be beaten.
But as long as hospitals can get away with underreporting errors or not reporting adverse events — as long as they cling to a “deny and defend” strategy instead of building a culture of respect, transparency, fairness and compassion — patients in the United States, Canada and elsewhere will remain at risk. And their families will continue to be plagued by the life-altering nightmare that hospital harm, and its aftermath, can inflict.
Medical errors are an epidemic that is clearly represents a public health crisis. It needs to be treated as such by lawmakers, healthcare policy makers, clinicians and the public.
The Center for Patient Protection believes that raising public awareness about the risks of hospital harm, while strengthening transparency and accountability on the part of hospitals in their handling of medical errors, is vital to making patients safer. We hope the information on these pages, gathered from discussions with hundreds of patients and families and a review of thousands of pages of patient safety literature, will motivate you to explore the issues further. If you are a hospitalized patient or family member, we hope you will be encouraged to become informed, engaged and protected as you navigate your healthcare journey.
(Originally posted 2015)
RELATED
Preventable Medical Error Is Canadian Healthcare’s Silent Killer
Informative Videos
U.S. Senate Hearings into Hospital Harm
PBS Segment on New Figures on Hospital Harm
Consumers Union on Hospital Care and Respect
ABC News on Surgery Errors
Hospital-Acquired Infections
HAI from the CDC
HAI in Canada
A Still-Grieving Mother Talks about Compassion and Transparency (TED Talk)
